Conference Report
| Rev Diabet Stud,
2008,
5(3):180-183 |
DOI 10.1900/RDS.2008.5.180 |
Intensive Glycemic Control and Macrovascular Disease in Type 2 Diabetes – A Report on the 44th Annual EASD Meeting, Rome, Italy, September 2008
Tapani Rönnemaa
Department of Medicine, University of Turku, FIN-20520 Turku, Finland, e-mail: tapani.ronnemaa@utu.fi
Manuscript submitted October 26, 2008; resubmitted November 2, 2008; accepted November 10, 2008.
Keywords: type 2 diabetes, glycemic control, UKPDS, myocardial infarction, macrovascular, hypoglycemia
Abstract
The impact of strict glycemic control on the prevention of macrovascular diseases in type 2 diabetes patients has remained unresolved for decades. New results presented at the EASD meeting shed new light on this question. Recent data from the United Kingdom Prospective Diabetes Study (UKPDS) showed that intensive glycemic control, when initiated immediately after diagnosis of type 2 diabetes and continued for a period of ten years followed by another ten years without special intervention, prevents myocardial infarction and decreases all-cause mortality. The Veterans Affairs Diabetes Trial demonstrated that striving to achieve near-normal glycemia in older patients with relatively long duration of diabetes and, in many cases, previous macrovascular events did not reduce future macrovascular events but increased the risk of severe hypoglycemia. These results indicate that effective treatment of hyperglycemia should be started early after diabetes diagnosis. However, introducing strict diabetes control after more than 10 years diabetes duration may lead to unfavorable effects in patients with hitherto unsatisfactorily controlled diabetes.
Introduction
At the 44th Annual Meeting of the European Association for the Study of Diabetes (EASD), several presentations addressed the question of strict glycemic control and macrovascular disease in type 2 diabetes. In June 2008, the results of two large intervention studies (both with over 10,000 participants), ACCORD (Action to Control Cardiovascular Disease in Diabetes) and ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) were published in the New England Journal of Medicine [1, 2]. Their results have caused concern as neither study showed any benefit with respect to macrovascular events in patients with intensive glycemic control.
ADVANCE study
Dr. Chalmers presented recent results from the ADVANCE study [3]. The study aimed to achieve HbA1c levels of 6.5%. In the intensive arm, therapy was based on sulphonylurea followed by insulin. Baseline HbA1c was 7.5% in both groups and the levels achieved were 6.5% and 7.3% in the intensive and control arms respectively. There was no difference in macrovascular outcomes after 5 years, but the coronary heart disease mortality curves tended to diverge at the end of the study to the benefit of the intensive group. The study also assessed the effect of strict hypertension control (perindopril + indapamide) on cardiovascular disease (CVD) outcomes: there was a 14% decrease in total and an 18% decrease in cardiovascular mortality in the active group. At the EASD meeting, the combined effects of strict glycemic and blood pressure control were presented: there was a 24% decrease in CVD mortality and an 18% decrease in total mortality in the combined (hypertension plus hyperglycemia) intensive treatment group. Statistical analyses revealed that the effects of blood pressure treatment and hyperglycemic treatment were additive and fully independent of each other.
Veterans Affairs Diabetes Trial (VADT)
Dr. Duckworth presented the results of the VADT (Veterans Affairs Diabetes Trial) study [4]. The baseline characteristics of the patients have recently been published [5]. The 1791 patients were in poor metabolic control with a mean HbA1c of 9.0% during maximum oral or insulin treatment. Duration of diabetes was 11 years and 40% of the patients had a positive history of CVD. Patients randomized to intensive glycemic control achieved an HbA1c level of 6.9%, whereas HbA1c in the conventional treatment group was 8.4%. Both groups were well controlled for hypertension and serum lipids and 95% had aspirin therapy. There was no significant difference between the groups in the primary outcome of major cardiovascular events. Severe hypoglycemia was observed in 21% and 10% of intensively and conventionally treated patients, respectively. Severe hypoglycemia was a strong predictor of primary outcome (RR 2.1, p = 0.018). There were 4 and 11 sudden deaths in the control and intensive treatment group (p = 0.07) respectively. It is possible that these events were associated with severe hypoglycemia. Duration of diabetes seemed to be critical with respect to the effect of intervention: intervention tended to increase the risk for CVD events in patients with diabetes duration > 15 years, while decreasing the risk in those with diabetes duration of less than 12 years.
United Kingdom Prospective Diabetes Study (UKPDS)
Drs. Holman and Matthews presented the new 20-year follow-up results of the United Kingdom Prospective Diabetes Study (UKPDS) [6]. These results were published after the EASD congress in the New England Journal of Medicine [7, 8]. The intervention period in the UKPDS ended in 1997. After the active intervention phase, the risk of myocardial infarction was 16% lower in the actively treated group, but the significance of this result was only borderline (p = 0.052). This has caused much debate for many years about the role of hyperglycemia treatment for the prevention of macrovascular disease in type 2 diabetes patients. After the intervention period, the patients were treated by their primary care physicians. The patients were seen by the investigators annually from 1997 to 2002 and thereafter followed up by questionnaires sent to the patients and their physicians. The overall mortality in 20 years was 44%. HbA1c values in intensively treated and conventionally treated groups were approximately the same from 1997 to 2007, although there had been a 0.9% difference in HbA1c between the groups in favor of the actively treated group during the intervention period. Among non-obese patients, the risk of myocardial infarction was reduced by 15% (p = 0.01) and total mortality was reduced by 13% (p = 0.007) in the active group. Among obese patients (allocated to metformin in the active group), the risk for myocardial infarction was decreased by 33% (p = 0.005) and total mortality by 29% (p = 0.002). The authors concluded that better glucose control in the intervention phase had a "legacy effect" on macrovascular complications, which corresponded to the effect previously observed in the DCCT/EDIT study in type 1 diabetes and designated “metabolic memory” [9].
The UKPDS study also examined the effect of intensive blood pressure lowering on cardiovascular events. During the active intervention period, systolic blood pressure was approximately 10 mmHg and diastolic blood pressure approximately 5 mmHg lower in the actively treated group, but during the follow-up period there was no longer any difference in blood pressure between the groups. The risk for myocardial infarction or total mortality was similar in the groups originally allocated to intensive or conventional blood pressure treatment. The authors concluded that the "legacy effect", observed in the treatment of hyperglycemia, was not observed in the treatment of hypertension.
Explanations for the apparent inconsistency between the UKPDS and other recent studies
Three recent studies (ACCORD, ADVANCE and VADT) suggest that strict glycemic control does not reduce macrovascular complications. In fact, in the ACCORD study, intensive glycemic control was associated with increased total mortality. In contrast, new results from the UKPDS indicate that better glycemic control reduces myocardial infarction and total mortality. How can this inconsistency between the studies be explained?
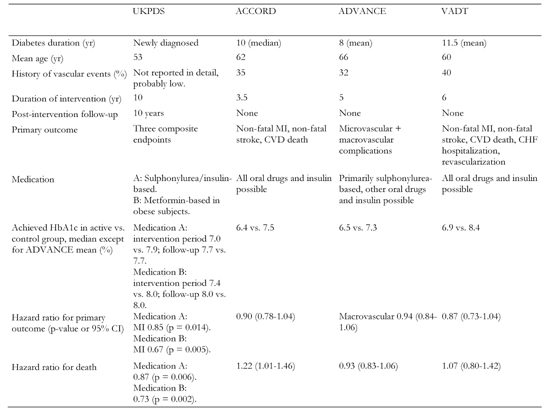
Table 1 compares the main characteristics of these four trials and provides several possible explanations for the discrepancy, many of which relate to differences in the study populations. Firstly, in UKPDS, the patients were newly diagnosed, whereas in the other three studies the mean duration of diabetes was 8 to11 years. Secondly, in the active group in the UKPDS, median HbA1c level was 7.0% during the intervention period and 8.0% thereafter, while in the active groups of ACCORD and ADVANCE the mean level was approximately 6.4% and 6.9% in the VADT. Thirdly, in the UKPDS, patients were principally free of cardiovascular disease at baseline, whereas in the other three studies a considerable proportion (32% to 40%) of the patients had already experienced a cardiovascular event. Fourthly, the incidence of severe hypoglycemia was lower in the UKPDS compared with the more recent trials. The fifth factor to be considered is that the UKPDS intervention period occurred, on the whole, in the prestatin era, whereas in the other studies statin use was very common, e.g. 80% of the patients in the VADT used statins. In theory, it is possible that the extensive use of statins, with their well established preventive effect on coronary heart disease events, may have masked the positive effects of effective hyperglycemia treatment. Finally, the positive effect of intensive hyperglycemia treatment in the UKPDS study achieved only borderline significance after 10 years of intervention and attained clear statistical significance 20 years from baseline, when a large number of cardiovascular events had occurred. On the other hand, the three other studies all ran for a considerably shorter time (3.5 to 6 years), which means that we will never know, whether a longer intervention period would have yielded a more positive result.
Table
1.
Recent trials examining the effect of glycemic control on macrovascular outcomes |
|
 |
 |
Legend:
Only macrovascular outcomes are included. UKPDS and ADVANCE also examined the effect of tight blood pressure control on vascular outcomes, but these aspects are not included in the table. MI: myocardial infarction. CVD: cardiovascular disease. CHF: chronic heart failure. |
|
Conclusion for clinical application
How should the results of these four studies be interpreted with respect to the treatment of hyperglycemia in type 2 patients? I feel that we should treat hyperglycemia actively as soon as diabetes is diagnosed. At this stage, the target HbA1c could remain at 6.5%, if achieved without hypoglycemia. On the other hand, older patients with longer duration of diabetes, patients with hypoglycemia unawareness or those with existing cardiovascular disease should have a higher HbA1c target of 7.0% or even higher, especially if they need complicated treatment with several oral drugs combined with insulin. Finally, as the Steno 2 trial [10] convincingly demonstrated, we should never forget that most effective prevention of macrovascular disease must always involve a multifactorial approach.
References
- Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008. 358(24):2545-2559. [DOD] [CrossRef]
- ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008. 358(24):2560-2572. [DOD] [CrossRef]
- Chalmers J. New results from the ADVANCE trial. Oral presentation at plenary session, 44th EASD Annual Meeting, Rome, September 2008. [DOD]
- Duckworth WC, Abraira C. Veterans Affairs Diabetes Trial. Oral presentation at plenary session, 44th EASD Annual Meeting, Rome, September 2008. [DOD]
- Abraira C, Duckworth WC, Moritz T. Glycaemic separation and risk factor control in the Veterans Affairs Diabetes Trial: an interim report. Diabetes Obes Metab 2008. In press. [DOD]
- Holman RR, Matthews DR. UKPDS 30 year data - are there legacy effects of improved glucose and blood pressure control? Oral presentation at plenary session, 44th EASD Annual Meeting, Rome, September 2008. [DOD]
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008. 359(15):1577-1589. [DOD] [CrossRef]
- Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med 2008. 359(15):1565-1576. [DOD] [CrossRef]
- Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B, Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005. 353(25):2643-2653. [DOD] [CrossRef]
- Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008. 358(6):580-591. [DOD] [CrossRef]
This article has been cited by other articles:
|